Jim Stratman, 69, knew from personal experience that chest pain should not be ignored. When he experienced persistent chest pain while traveling in Colorado, Stratman and his wife Sharon cut the trip short, returning home to see his cardiologist at Baylor Regional Medical Center at Grapevine. Before he could see his cardiologist, though, Stratman's blood pressure suddenly dropped. He went immediately to Baylor Grapevine's emergency department.
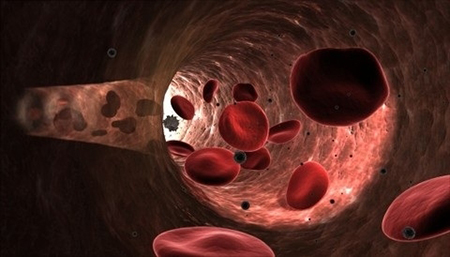
A series of diagnostic tests in the cardiac catheterization lab revealed an unusual and life-threatening heart attack mechanical complication called ventricular septal rupture: a tearing of the wall between the right and left ventricles, causing blood flow to pass between these heart chambers. There was a hole in his heart. Because of his progressive health deterioration and imminent risk of death, Stratman required immediate surgery.
"Post myocardial infarction posterior ventricular septal defect– the medical term for Mr. Stratman's condition – carries a mortality of 90 percent if this complication is not diagnosed expediently. In addition, there is about 50 percent mortality rate for this type of surgery," explained cardiothoracic surgeon Aldo Rafael. He is on the medical staff at Baylor Regional Medical Center at Grapevine and Baylor University Medical Center at Dallas. In consultation with Baylor Grapevine cardiologists, the two medical teams decided to transfer Stratman to Baylor Dallas.
Before transferring Stratman to Baylor Dallas, the Baylor Grapevine critical care team placed Stratman on extracorporeal life support or ECMO, a technique of providing cardiac and respiratory support oxygen to patients whose heart and lungs are severely damaged. Because of the critical nature of Stratman's condition, his heart needed rest. ECMO provided this rest, taking over the heart and lungs' functions by mechanically reoxygenating the blood outside the body.
Stratman was admitted to the intensive care unit (ICU) at Baylor Dallas. He remained on ECMO in ICU for three days before undergoing a six-hour surgery on August 1 to repair the hole.
During surgery, the surgeon first used Gore-Tex to patch the nickel-size hole in the heart septum (wall). Then he used part of a pig's membrane heart to cover the Gore-Tex patch. When surgery was completed, Stratman spent the next 30 days in the ICU.
Almost four months later, Stratman is home in Hickory Creek, Texas, ready to celebrate life and the holidays. From Baylor Dallas, he moved to Baylor Medical Center at Frisco where, in 11 days of inpatient cardiac rehab, Stratman progressed from being pushed in a wheelchair to walking around the hospital. Now he's in outpatient cardiac rehabilitation three days a week at Baylor Grapevine to gain strength, muscle tone, and endurance. "I really look forward to the class," says Stratman who admits exercise had not been a priority. "It's 45 minutes of really hard work."
Life is definitely better now than that day in late July. Stratman is regaining some of the 30 pounds he lost while hospitalized. His physician anticipates Stratman returning to a full life post-surgery. The normalcy of sharing every day with Sharon, taking vacations and driving his own car has helped put the summer's dramatic heart episode behind him. "I'm enjoying family and being alive," Stratman said.
Physicians are members of the medical staff at one of Baylor Health Care System's subsidiary, community, or affiliated medical centers and are neither employees nor agents of those medical centers or Baylor Health Care System.
MEDIA CONTACT:
Susan Hall
SusanH@baylorhealth.edu
Office: 214-820-1817
About Baylor Scott & White Health
As the largest not-for-profit health system in the state of Texas, Baylor Scott & White promotes the health and well-being of every individual, family and community it serves. It is committed to making quality care more accessible, convenient and affordable through its integrated delivery network, which includes the Baylor Scott & White Health Plan, Baylor Scott & White Research Institute, the Baylor Scott & White Quality Alliance and its leading digital health platform – MyBSWHealth. Through 51 hospitals and more than 1,200 access points, including flagship academic medical centers in Dallas, Fort Worth and Temple, the system offers the full continuum of care, from primary to award-winning specialty care. Founded as a Christian ministry of healing more than a century ago, Baylor Scott & White today serves more than three million Texans. For more information, visit: BSWHealth.com
